January 5, 2018
This is the third in a series of blog posts exploring the threat that drug resistance poses in fighting the epidemics of AIDS, tuberculosis (TB) and malaria. The full series is available here.
Today, an estimated 20.9 million people living with HIV/AIDS are on antiretrovirals (ARVs), up from 7.7 million in 2010. Although access to HIV treatment has grown dramatically, 15.8 million people living with HIV/AIDS are still not on treatment today. Getting people on treatment is not only important in allowing HIV-positive people to live full lives, but also because “treatment as prevention” is a key pillar in the global fight against the disease. Yet a recent Lancet article shows that an increase in ARV drug resistance is posing a significant threat to progress to date, and to our ability to end the epidemic.
HIV drug resistance arises from mutations in the virus’s genetic structure. These mutations, which can occur before or after treatment begins, can make the drugs used to treat HIV/AIDS less effective, or in some instances completely neutralized. The likelihood of drug-resistant mutations arising, increases as a result of multiple factors including poor drug quality and barriers to adherence to treatment plans.
There are a number of reasons that people living with HIV/AIDS may have difficulty in adhering to their treatment plans, including: side effects from medications, difficulty in covering costs, the stigma associated with HIV/AIDS, and stockouts of drugs. First of all, programs need to support those on treatment to surmount these barriers. Second, it is important to have HIV drug resistance surveillance systems in place. Surveillance systems can be instituted within national HIV monitoring and evaluation systems that are already in place in most countries, and allow countries to be more proactive in responding to observed increases in drug resistance.
A recent report by the World Health Organization (WHO), the Centers for Disease Control and Prevention, and the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) emphasizes the importance of national drug resistance surveillance systems and the urgency of responding to growing HIV drug resistance. Of the 11 countries that have reported data on pre-treatment HIV drug resistance (resistance detected before an individual begins taking ARVs), six countries reported resistance levels at or above 10 percent to the two most affordable and widely used drugs.
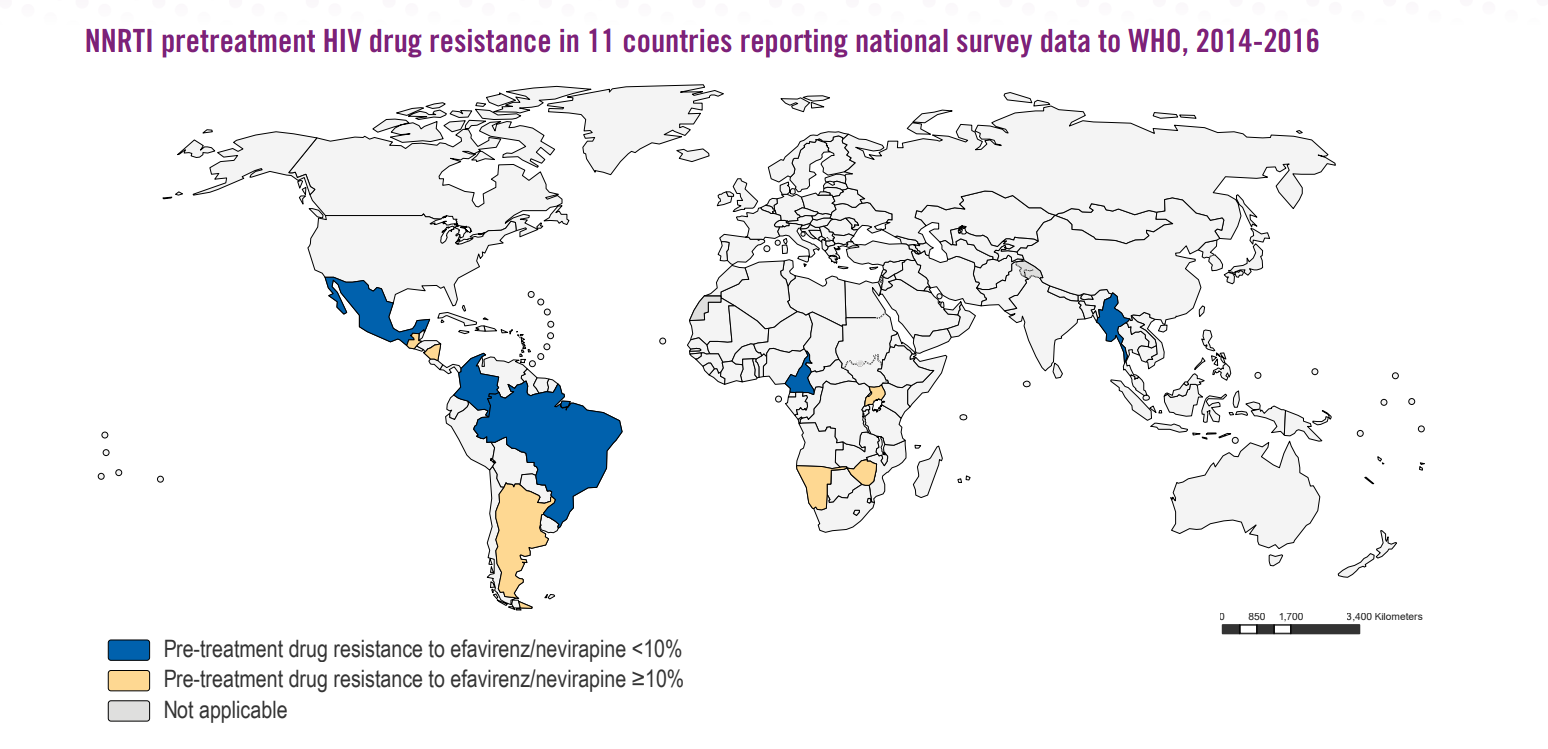
Source: World Health Organization
This 10 percent level is a critical measure. In UNAIDS’ “90-90-90” targets to support ending the AIDS epidemic by 2030, the final “90” calls for 90 percent of all people receiving ARVs to be virally suppressed. Among the obstacles to viral suppression, if drug resistance levels are over 10 percent, the 90 percent goal will be out of reach. In those cases, countries must consider a change from first-line treatment options to alternative medications that may be up to 14 times more expensive in order to meet this target.
Ultimately, if no action is taken to address the growing risk of HIV drug resistance, the WHO projects that there could be an additional 105,000 new infections, 135,000 deaths, and an increase of $650 million in treatment costs over the next five years.
With sufficient resources, the Global Fund has the ability to address drug resistance to TB and malaria – an effort that is key to countering the ballooning of medical, economic, and human costs that higher resistance would create down the road. The same is true of the HIV: with strategic investment, the Global Fund can build on its existing strategy of working hand-in-hand on Country Operational Plans and implementation with the U.S. President’s Emergency Plan for AIDS Relief, and place countries on the best possible footing to fight drug resistance in HIV.
